
Lets Understand stenosis
Lumbar canal stenosis is a condition where the channel running through the lower part of the spine (lumbar canal) becomes excessively narrowed (stenosis). Stenosis is due mainly to degenerative wear-and-tear, over many years, causing a thickening of the various bones, joints and ligaments that form the spinal canal. Degenerative changes are normal in adult life. They are more likely to cause the symptoms of lumbar canal stenosis, however, in someone who is born with a smaller than average lumbar canal. The narrowing usually affects one or two vertebrae, and sometimes can involve up to five “levels” in the lumbar spine.
Causes
- Arthritis
- Falls
- Accidents
- Wear and tear on the spine’s bones and joints

Symptoms
- Combination of back pain and symptoms in the legs.
- The symptoms in the legs indicate that there is pressure on the spinal nerves as they pass through the point(s) of narrowing in the lumbar spine, resulting in either sciatica (sharp pains shooting down the back of one or both legs), or claudication (heavy, dull aching, with pins and needles in the feet and legs brought on by standing or walking).
- These symptoms usually start when you are standing or walking. Often, the symptoms get better if you sit, crouch or lie in the fetal position (on your side with your knees tucked up to your chest).
- It’s thought that these positions “open” the lumbar canal and take the pressure off the nerves that go to the legs.
- In severe cases, stenosis can cause partial or complete bowel or bladder incontinence.
Diagnosis
The diagnosis can be made with a CT scan or MRI scan of the lumbar spine.An MRI scan is a simple and safe test, similar in many ways to a CT scan. MRI use a technique known as magnetic resonance imaging. No radiation is involved. There is no need to be admitted to hospital and usually no need for injections, although people prone to claustrophobia may find the examination stressful and should discuss their anxiety with medical staff at the time of the test. People with heart pacemakers cannot have an MRI.

Prevention Plan
For six weeks when you get home, the most important thing to do is rest. Your wound needs time to heal, internally as well as externally. Avoid undue bending and lifting. Minimise sitting to essentials such as eating and toileting. It is advisable to avoid driving, and even sitting as a passenger, in a car.
Schedule two good walks of about 15 minutes each per day. Swimming is excellent exercise after spinal surgery but you should wait to begin until after your post-operative review, which is usually six weeks after surgery.
In most cases, the symptoms caused by the disc prolapse will have eased within six weeks of surgery but this varies greatly from person to person.
At Physioline, all the members of the rehabilitation team work together so as to provide proper care and the therapy in order to
- Pain relief
- Muscle strengthening
- Traction
- Positioning
- Correction of posture
- Prescription of splint

Treatment Goals
- Reduce nerve compression
- Restore the level of function you had before the injury.
- Limit loss of function
- Prevent injury or more damage to other structures.
- Reduce pain
- Prevent complications.
Combination Therapy is the ONLY Answer for Spinal Restoration
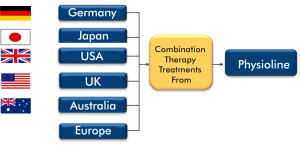
Why You must come to Physioline?
- Achieve Breakthrough Results.
- Fastest recovery time in India.
- Combination Therapy Usage for the first time in India.
- 17 years of Experience in Combating Pain.
- World-class Technological Advances under one roof.
Highlights of Our Treatment
- Innovative Programs to prevent Surgery.
- Unique treatment Approach for the first time in India.
- Continuous Up gradation of Professional skills and techniques.
- Patients could avoid surgical intervention in the past.
- Spinal Restoration implemented for medical tourism patients for the first time in India.
- Highest Success Percentages achieved in India.
Innovation with Expertise

Unmatched treatment Protocols for first time in India

Most Advanced Technological Advances in India

We assure complete Recovery with pain Free Life Always..

Videos Testimonials
Success Stories
I don't have the words to thank Indicure and Physioline, who have made a remarkable change in my life. I had this perpetual pain in shoulder and back, which had made my life terrible. I had tried various treatments but to no use. I then learnt about this center in Mumbai and decided to go there. Now, I feel so much healthy and full of life. Thanks everyone at Indicure and Physioline.Miss C.Tonsing , Nepal Cervical Spondylosis (C5-C6) with radiating pain to right arm---Physiotherapy and Rehabilitation
I am very much thankful to” PHYSIOLINE” for giving me the best Physiotherapy treatment. I was in severe pain as I was suffering from Cervical Spondylosis, I was unable to carry out my daily activities at home & at work. After undergoing the treatment at physioline I am feeling much better.Miss Chaya, INDIA CERVICAL SPONDYLOSIS
I am extremely thankful to Dr. Sanjay Bakhshi and his entire team at physioline for changing my life. I had begun to think that I would never ever get rid of the pain in both my knees. I used to get severe pain in my knees while climbing up & coming down the stairs but after taking physiotherapy treatment at PHYSIOLINE my pain subsided within a short period of time.Mrs Rekha Raval Bilateral Osteoarthritis---Both Knees
