We can improve quality and longivity of life
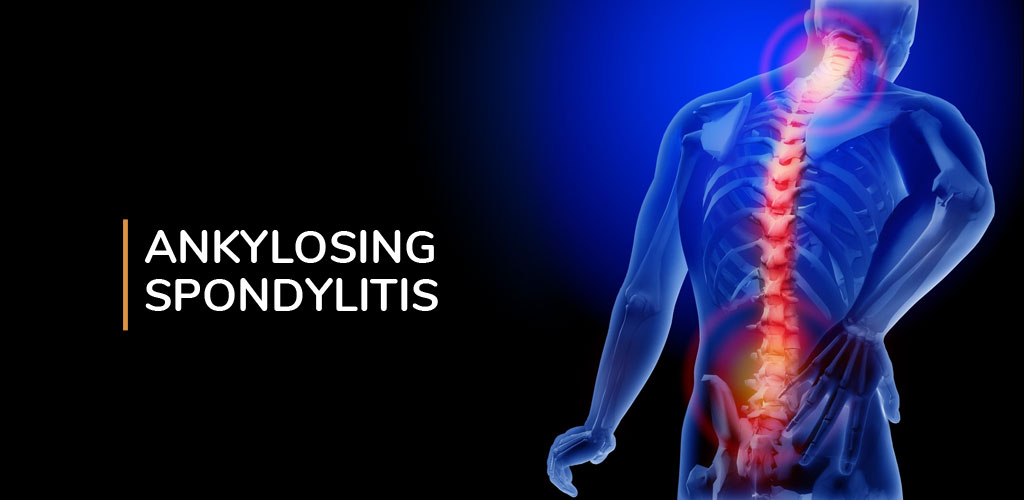
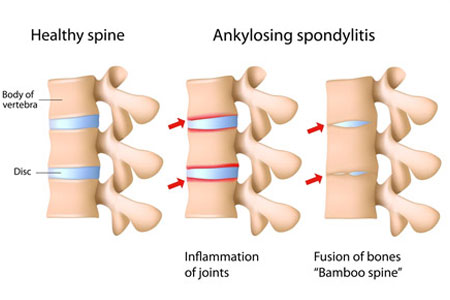
Ankylosing spondylitis is a form of chronic inflammation of the spine and the sacroiliac joints. Chronic inflammation in these areas causes pain and stiffness in and around the spine. Over time, chronic spinal inflammation (spondylitis) can lead to a complete cementing together (fusion) of the vertebrae, a process referred to as ankylosis. Ankylosis leads to loss of mobility of the spine.
Ankylosing spondylitis is also a systemic rheumatic disease, meaning it can affect other tissues throughout the body. Accordingly, it can cause inflammation in or injury to other joints away from the spine, as well as other organs, such as the eyes, heart, lungs, and kidneys.
Causes
- Genetically inherited, born with the HLA-B27 gene.
- Chronic tissue inflammation resulting from the continued activation of the body’s own immune system in the absence of active infection is the hallmark of an inflammatory autoimmune disease.

Signs & Symptoms
- Inflammation of the spine, joints, and other organs.
- Fatigue
- Pain and morning stiffness of the spine and sacral areas with or without accompanying inflammation in other joints, tendons, and organs.
- Expansion of the chest with full breathing can be limited because of rigidity of the chest wall.
- Severely affected persons can have a stooped posture. The symptoms of pain and stiffness are often worse in the morning, or after prolonged periods of inactivity.Patients who have chronic, severe inflammation of the spine can develop a complete bony fusion of the spine (ankylosis).
DIAGNOSIS
- Patient’s symptoms
- Physical examination
- X-ray finding
- Blood tests
- Tests for Rheumatoid factor and antinuclear antibodies
- pulmonary function studies

Combination Therapy is the ONLY Answer for Spinal Restoration

Why You must come to Physioline?
- Achieve Breakthrough Results.
- Fastest recovery time in India.
- Combination Therapy Usage for the first time in India.
- 17 years of Experience in Combating Pain.
- World-class Technological Advances under one roof.
Suggestions for lifestyle modifications that may help AS patients better control the symptoms of the condition include
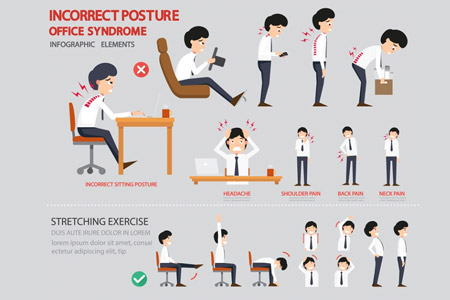
Workplace Modifications
- Most patients with ankylosing spondylitis continue to be employed full-time. Improve or modify your work environment for optimum positioning of your spine and good posture. These can be achieved by modifications such as:
- Pay attention to your habitual posture while standing or sitting and make a mental (or written) note to yourself of how to modify it for better spinal alignment.
- Adjust your chair at your desk so that you do not bend forward to work
- Try not to stand in one position for a long time. If you must stand in one position for an extended period of time, try to move as many joints as possible while standing such as wiggling your toes and stretching your shoulders.

Home Modifications
- At home, modify your behavior and surroundings to maintain good posture and to reduce situations that may exacerbate pain. Suggestions include:
- Every effort should be made to keep the spine straight.
- When sitting for long periods of time (e.g., watching TV, eating a meal, reading), stretch your spine by straightening your posture and pulling your shoulders back
- Try to sit in a chair with a firm seat, an upright and tall back, and armrests to relieve the weight from your spine. Soft chairs and sofas tend to exacerbate back pain and stiffness by being conducive to bad posture.
Sleep Modifications
- Some relatively minor modifications may help you get a better nights sleep and reduce the extent of fatigue that you may experience in the daytime. Some helpful suggestions include:
- Sleep in a bed which is firm but not too hard.
- Sleep on one pillow if possible and support the hollow of the neck. Multiple pillows increase the angle of bend in the cervical spine (neck).
- If you need to sleep on your stomach, try to do so without a pillow under your head and let your feet dangle off the end of the bed.
- Try not to sleep in a curled position but rather keep your legs straight


General Lifestyle Modifications
- Take a warm shower or bath in the morning if stiffness is a problem. Some people find it helpful to do stretching exercises while standing under hot water in the shower.
- For specific areas of inflammation, try applying hot packs or ice.
- Avoid wearing a corset or brace or any garment that keeps the spine rigid since it is very important for the patient with AS to move and exercise the spine to relieve or avoid stiffness.
Innovation with Expertise

Unmatched treatment Protocols for first time in India

Most Advanced Technological Advances in India

We assure to improve your quality of Life
Videos Testimonials

Success Stories
Treatment all together was the best and a quality treatment as a package. Doctors have done a commendable job. The staff was also very helpful. Thanks a lot to the whole team of Physioline.specimen book.Mr.Shivam Mistry Neck Pain radiating to hands and jaw pain.
My overall experience at Physioline was very comfortable. The pain has also reduced and I have learnt a lot about exercises, postures, and also a lot about reducing back pain. If I do all the recommended exercises I am pretty confident that I will recover fully.i would surely recommend anyone suffering with lower back pain to please go to Physioline. The best part is the effectiveness of the equipment .book.Mr.Navin Sai Madiraju Lower Back Pain
My constant neck pain has gone. All the treatment that I received here ay Physioline was excellent and great. I am so thankful to Dr.Sanjay Bakhshi and the entire team of Physioline to give me such an amazing world class treatment which helped me avoid surgery. I am honestly so relieved that I feel so much better now.I highly recommend all the people suffering from the same problem (cervical spondolities) as me to come here at Physioline and get a non-surgical treatment . Thanks for making my pain go away and my future bright. Wish you all the best and success in helping people and may your clinic be well recognized all over the world.ok.Mrs.Mamta Vikas Sawant Neck Pain
As regards my shoulder pain, compared to earlier has reduced a lot.Dr.Sanjay Bakshi & his team of doctors were excellent and supportive in every matter.The services provided were very good and the co-operation extended especially my timing adjusted very well.Since I stay in four bungalows I felt safe and comfortable to move around as this place was very familiar to me.The environment in Dr.Bakshi”s clinic was also neat ,clean and hygienic.I shall definitely do my exercise without fail everyday given by Dr .Sanjay Bakshi.Mrs.Genevieve Sylvia Pinto Cervical Pathology With Shoulder Pain.
